The annual Amarnath Ji Yatra (pilgrimage) from 2011 to 2012 reported 231 deaths. While one might assume bad weather or natural disasters were responsible, the real cause was far more preventable. Unfortunately for these Lord Shiva devotees, cardiac and pulmonary issues were among the chief causes of death, proving that “Ignorance is not bliss,” especially at high altitudes.
Among many altitude-related illnesses, HAPE (High Altitude Pulmonary Edema) was observed in the 31 pilgrims treated at a medical center in Kashmir. Even with medical support, the survival ratio stood at 28:3.
An early diagnosis and following the authorities might have saved the casualties. It wasn’t the first time for a misdiagnosed HAPE; it has been so for centuries till the first autopsy report on HAPE surfaced in 1891. Before Dr. Jacottet’s unfortunate death at Mt. Blanc, HAPE was mistaken for pneumonia that young men often catch at high altitudes.
The dismissive attitude is left far behind by science, but the laymen still emphasize carrying the baton forward. Not understanding the risks of just a mild dry cough takes you closer to a mortality rate of up to 50%. The real problem? Little to no public awareness. And it is followed by an inability to recognise the symptoms and respond to them aptly.
This article will serve as an eye-opener for anyone who’s looking to trek beyond an altitude of 2,500 m. Through you, we aim to create awareness for a safer and healthier trekking experience. Read it thoroughly and ask if in doubt!
Note: Your awareness could save not only your life but that of a fellow trekker. If they can’t see the risks, be their voice of reason.
Table of Contents
What is High-Altitude Pulmonary Edema (HAPE)?
A very simplified definition for HAPE is, “HAPE is a severe form of acute mountain sickness (AMS) observed within 2-5 days of being at an altitude >2500 m.” Then the question that remains is, why did something as ‘mild’ as AMS deserve such a dramatic SOS? This question leads us to our next definition, which states,
“HAPE may appear similar to AMS at first. But as it progresses, fluid begins to fill the lungs due to low oxygen levels in the blood. This leads to difficulty breathing (dyspnoea), poor exercise performance, and a dry cough. If untreated, it can cause irreversible damage, and even death.”
A more medically relevant definition for HAPE states,
“High-Altitude Pulmonary Edema (HAPE) is a non-cardiogenic pulmonary edema caused by hypoxia-induced, uneven pulmonary vasoconstriction. This leads to high capillary pressures, blood–gas barrier disruption, fluid leakage into alveoli, impaired fluid clearance, inflammation, oxidative stress, and reduced nitric oxide bioavailability, collectively resulting in pulmonary edema and impaired gas exchange.”
Quick Help with Medical Jargon:
| Term | Meaning |
| Pulmonary edema | Fluid buildup in the lungs that makes breathing difficult |
| Non-cardiogenic | Not caused by heart problems |
| Hypoxia | A condition where the body or part of it doesn’t get enough oxygen |
| Hypoxemia | Low oxygen levels in your blood. |
| Polycythemia | Too many red blood cells are circulating. |
| Hypokalemia | Low potassium levels in your body. |
| Pulmonary vasoconstriction | Narrowing of the lung blood vessels due to low oxygen |
| Blood-gas barrier | The thin wall in the lungs where oxygen passes into the blood and waste gases exit |
| Oxidative stress | Damage from unstable molecules (free radicals) |
| Nitric oxide bioavailability | The amount of nitric oxide available to help relax and open blood vessels |
Types of HAPE

HAPE has subtypes, but we cannot consider these parallel to cancer stages or classifications. These subtypes, although they appear in different scenarios, share the same symptoms and require similar treatments. Here are the 3 types of HAPE you should know about:
- Normal HAPE: Seen in lowlanders coming for sojourns (temporary stay) to altitudes higher than 2,500 m. It usually shows effect within 2-5 days at that altitude. The mortality rate for this type is 11% and can go as high as 50% if left untreated (Paralikar, 2012).
- Re-Entry HAPE: Seen in highlanders returning from sojourns or long stays at a low altitude. It usually shows effect within 2-5 days at that altitude (Baniya et al., 2017). No studies have been conducted on their mortality and survival rates. Considering their symptoms and presentation, we can safely presume that they are a match to Normal HAPE.
- Delayed-onset HAPE: This type was highlighted in a study in the Ladakh region of Jammu and Kashmir, where eight patients were observed. They had developed HAPE after 6 days of a healthy stay at that altitude (11,500 ft). The mortality rate was as high as 50% (Singhal & Alasinga, 2020), despite receiving standard treatment.
Note: Regardless of the type, early recognition and treatment remain critical to survival.
What Causes HAPE?
There are two perspectives you can use to contemplate this question: internal and external. The internal refers to physiological responses, such as hypoxia, while the external involves factors like rapid ascent. The key difference lies in how each is applied. Understanding one can help prevent HAPE altogether, while understanding the other helps detect it early and take appropriate action. Below are the two with an extra anecdote:
Primary Internal Causes of HAPE (Physiological & Molecular Changes)
These are the core mechanisms responsible for fluid buildup in the lungs:
- Exaggerated pulmonary vasoconstriction
- Elevated pulmonary artery pressure
- Pulmonary hypertension
- Capillary wall leaks (stress failure)
- Mean pulmonary artery pressure > 35 mmHg (Paralikar & Paralikar, 2010)
- Systolic pulmonary artery pressure > 50 mmHg (Luks & Swenson, 2007)
- Low pulmonary artery occlusion pressure
- Increased sympathetic activity in the pulmonary vasculature
- Reduced cardiac output
- Decreased nitric oxide production
- Elevated endothelin-1 levels
- Inflammation of pulmonary vessels (Broaddus et al., 2016)
Impaired Fluid Clearance in the Lungs
These explain why fluid remains in the alveoli, contributing to edema:
- Diminished alveolar fluid reabsorption capacity
- Inhibited Na⁺ transporters
- Decreased transepithelial sodium transport
Primary External Causes of HAPE (Environmental/Behavioral Factors)
These are situational causes that worsen or trigger internal responses:
- Rapid ascent without acclimatization
- Cold ambient temperatures
- Vigorous or unaccustomed exercise at altitude
- Use of sleep medication or respiratory depressants
- Concomitant or persistent respiratory infections
- Unacclimatized exertion during initial altitude exposure
Other Risk Factors (Contributing Elements)
These increase susceptibility, but are not direct causes:
- Previous lung disorders
- Decreased air entry in the lungs
- Sickle cell disease
- Atrial septal defect / Patent foramen ovale (PFO)
- Intracardiac shunts
- Diabetes Mellitus
- Chronic Alcoholism
- COPD (Chronic Obstructive Pulmonary Disease)
- Hypokalemia (low potassium levels)
- Being male
- Blood vessel abnormalities
Symptoms to Identify HAPE
HAPE is harder to distinguish from AMS (Acute Mountain Sickness) in its early stage and escalates rapidly if untreated. Dismissal of symptoms as the body’s reaction to high altitude is a common concern. Patients may look better than they are, masking the underlying severity.
This disconnect is due to hypoxemia (abnormally low blood oxygen). SPO₂ levels at high altitude can drop to 40–70%, which would be critical at sea level. However, because SPO₂ naturally runs ~10% lower at high altitudes, trekkers often shrug it off as part of acclimatization.
Distrust in your body’s indicators can swiftly lead to fatal consequences. Early recognition is everything. Here’s what to watch for:
| Category | Symptoms |
| Most Common/Early Signs | Subtle non-productive cough, dyspnoea on exertion, acute-onset breathlessness, decreased exercise tolerance fatigue, headache, Nausea, Dizziness, Vomiting (non-specific, but reported), Chest discomfort, Elevated nocturnal heart rates, Prolonged recovery after exertion, Low-grade fever (elevated body temp not exceeding 38.5°C) |
| Moderate to Severe | Dyspnoea at rest, Orthopnea, Cyanosis, Tachypnea, Tachycardia, Chest congestion, Decreased air entry in both lungs, Bilateral crepitations/rales (On chest auscultation), Discrete rales in the mid-lung field (asymmetrical rales) |
| Severe/Later Stages | Gurgling in the chest, Pink frothy sputum (blood-tinged, productive cough) (Cremona et al., 2002). Slurred speech, Frothy secretions (may obstruct airways), Encephalopathy, HACE (14% chance) (Thareja et al., 2025) |
HAPE: Diagnostic Clues from Clinical Symptoms
We’ve already discussed the physical symptoms caused by HAPE. Now, here’s a list of clinical signs that frequently appear in HAPE patients during medical diagnosis:
| Category | Findings (Clinical Symptoms) | Tests/Tools Used | Diagnosis It Supports |
| PhysiologicalIndicators | Reduced cardiac output | Echocardiography / Cardiac monitoring | Right heart strain or altitude-induced dysfunction |
| Lower stroke volume | Echocardiography | Diminished preload/output due to pulmonary hypertension | |
| Ventilatory control instability | Clinical observation / Polysomnography | Disrupted breathing rhythm due to hypoxia | |
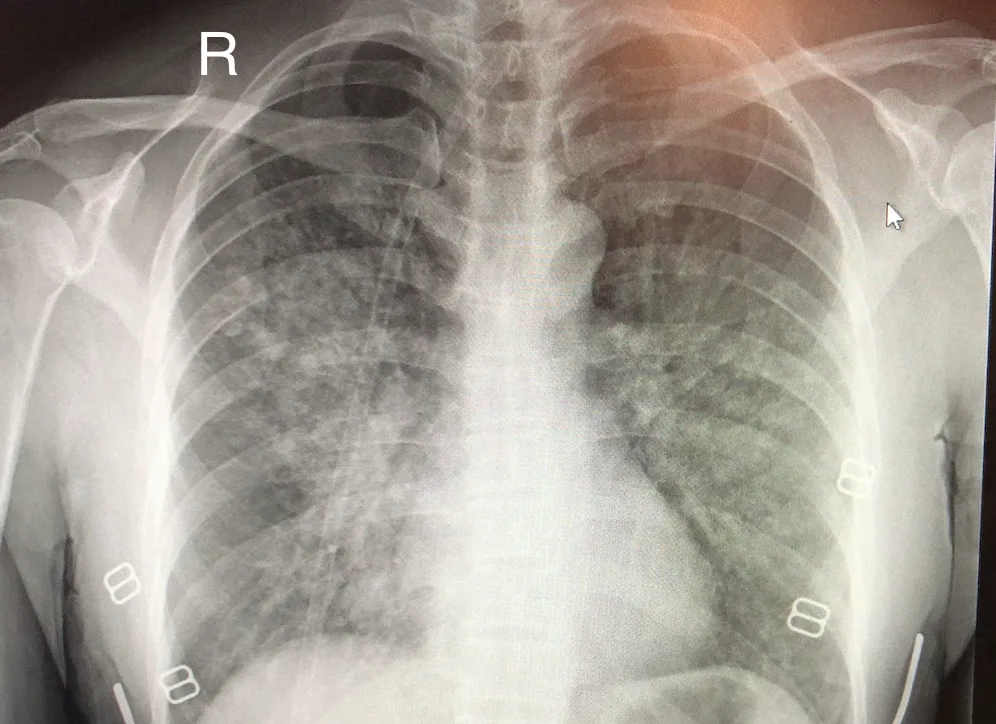
| Imaging | Patchy opacities on thorax imaging | Chest X-ray / CT | Non-cardiogenic pulmonary edema (HAPE) |
| Infiltrates in the right middle lobe | Chest X-ray / Lung Ultrasound | Early/interstitial pulmonary edema | |
| Bleeding in the lungs | Chest CT / Bronchoscopy / Sputum analysis | Pulmonary hemorrhage in advanced HAPE | |
| Lab | Polycythemia | CBC with Hematocrit | Chronic hypoxia due to altitude |
| Hypoxemia | Pulse Oximetry / ABG | Core feature of HAPE | |
| Hypokalemia | Serum Electrolytes (BMP/CMP) | Electrolyte disturbance secondary to hypoxia/fluid shifts | |
| PMN (Polymorphonuclear leucocytosis) | CBC with Differential | Inflammatory response (non-infective); helps rule out pneumonia |
Note: The above findings, tests, and diagnoses are not fixed standards. A physician can make a differential diagnosis after examining the combination of findings and their effects on an individual’s body. Therefore, the final diagnosis differs on a case-by-case basis. This table is a preliminary guide, not a substitute for medical training or judgment. It won’t make you a physician overnight.
HAPE vs Other Mountain Sicknesses: Differentials
What sets HAPE apart from other altitude illnesses is its persistence.
Most cases of Acute Mountain Sickness (AMS) improve within hours after taking acetazolamide. AMS, once resolved, permits continued ascent without descent (Luks et al., 2010); this is not the case with more severe altitude illnesses. If symptoms persist or worsen, it may no longer be AMS. It’s likely HAPE or HACE.
The two are easy to confuse; they affect very different systems:
- HAPE affects the lungs, causing breathlessness, coughing, and low oxygen levels. (Early Stages)
- HACE affects the brain, causing confusion, poor coordination, and behavior changes. (Early Stages)
Even the treatment differs:
- Nifedipine helps in HAPE (Maggiorini, 2006).
- Dexamethasone is key for HACE (Walsh & Agrawal, 2024).
Recognizing the difference can save lives.
Quick Rule of Thumb:
AMS = Reversible with acetazolamide
HAPE = Lung distress + needs nifedipine
HACE = Brain fog + needs dexamethasone
Who is at risk of developing HAPE?
HAPE is not some rare genetic disorder, and can happen to anyone; your high fitness levels are of no use. This makes it difficult to surely segregate the individuals who will develop HAPE from those who won’t. Although there’s no specific criterion to do so, we have identified some reported underlying conditions that increase the likelihood of contracting HAPE in a patient. Individuals with the following traits or conditions are more vulnerable to developing HAPE:
Physiological Predispositions
- Stronger-than-normal pulmonary vessel constriction at high altitudes
- Higher pulmonary artery pressure, even during sea-level exercise
- Increased sympathetic nervous system activity at altitude (Johnson et al., 1981)
- Low nitric oxide levels reduce vessel relaxation
- High endothelin-1 levels, tightening of lung vessels (Modesti et al., 2006)
- Smaller lung volumes, limiting oxygen uptake
- Poor lung diffusion response during exertion or low oxygen levels
- Reduced ability to clear fluid from the lung tissues
- Blunted ventilatory response to low oxygen (low HVR)
- Weak hormonal sodium balance during altitude exposure (blunted natriuretic response) (Swenson, 2010)
Pre-existing Medical Conditions
- Previous lung disorders
- COPD (Chronic Obstructive Pulmonary Disease)
- Sickle cell disease
- Diabetes mellitus
- Chronic alcoholism
- Hypokalemia (low blood potassium)
- Congenital heart defects (e.g., PFO or atrial septal defect)
- Intracardiac shunts
- Blood vessel abnormalities
History & Demographics
- Previous history of HAPE
- Being male (statistically higher risk) (Burtscher, 2021)
- Low ventilatory response at altitude
- Unfit or unacclimatized individuals during the first exposure
HAPE Susceptibility Check & Prevention
“Fake it till you make it” might work in life, but not at altitude. With HAPE, that mindset can cost you your life. If you’ve had HAPE before, your recurrence risk jumps to 60% (Deweber & Scorza, 2010). But even if you haven’t had HAPE before, certain physiological markers can reveal whether you’re at risk. These include:
| Check/Test | What it Indicates | When/How to Test |
| ↓ Nitric oxide & nitrate/nitrite in BAL fluid (Maggiorini et al., 2006) | Impaired vasodilation in the lungs during hypoxia | Bronchoalveolar lavage after hypoxic exposure |
| ↑ Endothelin-1 levels | Higher vasoconstriction predisposes to HAPE | Blood/plasma biomarker analysis |
| ↑ Systolic pulmonary artery pressure (sPAP) (Mounier et al., 2011) | Pulmonary arteries overreact to low oxygen | Doppler echocardiography during hypoxic exercise |
Prophylactic Treatment (Physician-Guided Only)
These susceptibility checks are only worth pursuing if approved by a physician. Once confirmed, your doctor may prescribe chemoprophylaxis, which is often tailored to individual risk. The most widely studied and used prophylactic medications for HAPE are:
- Nifedipine (30 mg SR, every 12 hrs or 20 mg, every 8 hrs): Oral (Bärtsch et al., 1991)
- Dexamethasone (4mg, every 6 hrs): Oral (Schoene, 2008)
- Tadalafil (10 mg twice/day): Oral
- Sildenafil (50 mg every 8 hrs): Oral
- Salmeterol (125 μg twice/day): Inhaled
- Acetazolamide (dosage varies): Oral (Kutzman & Caruso, 2018)
When to Start & Stop Prophylaxis?
Here are the points to keep in mind:
- Start your prophylactic medication on the day of ascent.
- Continue until the 3rd or 4th day after reaching your final sleeping altitude, whether it’s above or below 3000 m.
- Even if you feel acclimatized early, do not stop meds prematurely. (Bärtsch et al., 2003)
How to Prevent High Altitude Pulmonary Edema?
You’ve all heard it millions of times; here it repeats, “Prevention is better than cure.” For trekkers and explorers (both new and experienced), the thrill of reaching the summit should never outweigh the need for self-preservation. For a safe and successful high-altitude journey, you should learn how to pace yourself and stay one step ahead of altitude illness, whether it’s AMS, HAPE, or HACE. Below are the five steps to prevention:
Step 1: Ascend Gradually
Dozens of research studies later, one recommendation stood the test of time: After 2,500 m altitude, the ascent rate/day shouldn’t be more than 300-350 m, or at least the sleeping altitude shouldn’t be increased more than that number.
Rapid ascents, particularly by airlift to altitudes above 5,500 m, spike HAPE risk from 2.5% to 15.5% (Singh et al., 1965). One large Chinese study found that 56% of 11,182 lowland workers who quickly ascended to 3,500 m developed AMS. Notably, 50% – 70% of HAPE cases also present with AMS (Berger et al., 2020), making it a significant potentiating factor.
First Line of Defense: Climb high, sleep low.
Step 2: Prioritize Acclimatization
We’re often in a rush, male trekkers more than their female counterparts. Unfortunately, HAPE doesn’t favor the impatient. Studies show that men are more affected than women, reinforcing one truth: taking it slow matters.
The human body is made to adapt, not in a snap, but in ample time. As a lowlander climbing above 2,500 m, give your system the time it needs. Your trek itinerary should include at least 1–2 acclimatization days, depending on terrain and difficulty.
First Line of Defense: Give your body time to adjust.
Step 3: Avoid Overexertion
Let’s circle back to a core truth: this isn’t a race. In high-altitude trekking, slow and steady isn’t just safe, it’s survival. As Khan (2012) writes of the Siachen border, “Every day is a new day beyond 18,000 ft.”
Strenuous effort is a known risk factor for HAPE, as it triggers an exaggerated sympathetic response, which worsens your body’s Hypoxic Ventilatory Response (HVR), as described by Jensen and Vincent (2023). The result? Impaired oxygen delivery and the dangerous buildup of edema in the lungs.
The fix is simple: trek at your own pace. Overexertion isn’t one-size-fits-all. Listen to your body, recognize your limit, and know when to call it a day.
First Line of Defense: You’re not racing the mountains.
Step 4: Stay Warm & Well-Hydrated
High altitude is unforgiving. There’s a lack not just in oxygen, but also in temperature, as well, and we cannot forget the dryness. Cold exposure is a silent aggravator. It increases pulmonary artery pressure, tightening blood vessels and pushing fluid into the lungs. Add to that: dehydration, which thickens blood and stresses circulation, creating the perfect storm for HAPE.
Prevention is simple. Dress in layers, stay dry, and sip water regularly. Even if you’re not thirsty. Your body loses moisture faster at high altitude than you realize.
First Line of Defense: Cold and dry kills quietly.
Step 5: Know Your Body & Risks
Trekking? Fun. Ignoring your health history to trek? Dangerous.
The study on Amarnath Yatris found that 20 out of 31 HAPE patients had elevated levels of immune cells with granules. They’re often linked to infections, allergies, or asthma. These underlying conditions silently amplify your risk at altitude.
Before heading out, review your medical history. If you’ve had lung issues, heart defects, or HAPE before, consult a doctor. Prevention may even include prophylactic meds like nifedipine.
First Line of Defense: Know your limits before altitude does.
HAPE Treatments
Without timely care, the odds of survival drop drastically for a patient with HAPE. Naturally, early and aggressive management becomes the top priority to avoid irreversible consequences. Treatment for High-Altitude Pulmonary Edema broadly falls into three categories:
When Descent is an Option
(Primary Goals: Rapid descent + oxygenation)
A graded ascent of 600 m/day reduces the risk of HAPE to a mere 4%. This shows that altitude gain and resultant hypoxemia are the reasons for contracting HAPE. Therefore, losing altitude and supplemental oxygen becomes of utmost importance. Any trekker or mountaineer’s saving grace, in the absence of any medical care, is:
- Step 1 (1000 m Immediate Descent + Oxygenation): Maintains SpO2 >90%, which reduces hypoxemia and alleviates edema formation (Taylor, 2011).
- Step 2 (Maintain normothermia, i.e., normal body temperature): Prevents hypothermia-induced sympathetic surge that raises pulmonary artery pressure.
- Step 3: (Passive Descent on a Portable Stretcher): Prevents exertion-induced hypoxia, thereby minimizing further edema formation.
Note: The hyperbaric chamber and nifedipine therapy are handy if a 1000 m descent is not possible at the time or the situation doesn’t seem to improve as rapidly.
When Descent is Not an Option
(Primary Goals: Stabilize, simulate descent, reduce pulmonary pressure)
With Himalayan Dream Treks in Uttarakhand and Himachal, “Descent is ALWAYS an option.” But nighttime or weather-induced delays can make descent temporarily impossible.
So, what should you do when descent isn’t an option?
A study highlights that when it takes 2–3 days to reach lower altitudes, nifedipine becomes the cornerstone of HAPE management. At elevations around 4,559 m, sustained-release nifedipine 20 mg every 6 hours significantly alleviates symptoms (Oelz et al., 1989). Another study recommends dexamethasone as a steroid cover for HAPE. (Maggiorini, 2006).
But, in a broader sense, we have the following options:
- Option 1 (Adjunctive Pharmacologic Therapy): The administration of pharmacological agents like nifedipine, phosphodiesterase-5 inhibitors (sildenafil and tadalafil), dexamethasone, acetazolamide, β-agonists (salmeterol or albuterol), etc. You can get some clarity on their dosage and usefulness in the table below:
| Drug/Agent | Route | Dosage | Remarks |
| Nifedipine (Sustained Release) | Oral | 20 mg every 8 hrs or 30 mg every 12 hrs | Graded 1C by ACCP standards if descent is delayed. Lowers pulmonary artery pressure effectively. |
| Dexamethasone | Oral/IV (Intravenous) | 8 mg initially, then 4 mg every 6 hrs | Anti-inflammatory. Reduces vascular leakage. Useful when hypoxia persists. |
| Phosphodiesterase-5 inhibitors (Sildenafil/Tadalafil) | Oral | Varies | Potent pulmonary vasodilators. Strong physiologic rationale but limited clinical trial data. |
| Acetazolamide | Oral | Varies | Promotes acclimatization. Not curative for HAPE. |
| β-Agonists (Salmeterol/ Albuterol) | Inhaled/Nebulised | Varies | May improve airway clearance. Not proven to reverse pulmonary hypertension. |
Note: Acetazolamide, β-agonists, and phosphodiesterase-5 inhibitors are best seen as rescue or last-resort options, i.e., “Hail Mary” therapies. Don’t rely on them, especially if nifedipine is accessible.
- Option 2 (Hyperbaric Chamber or the Gamow Bag): Portable hyperbaric chambers work great in situations where descent sounds impossible, as they stimulate descent. It simulates descent by increasing ambient pressure (typically 2 to 4 lb/in², equivalent to a descent of about 1,500 meters). Use it as a temporary fix only.
Caution: Its effectiveness drops in the following conditions:
- Vomiting or persistent nausea
- Claustrophobia
- Altered mental status
- High risk of recurrence post-exit
- Option 3 (Normative Procedure): Unavailability of descent doesn’t entirely paralyse the standard treatment. Therefore, you are still supposed to:
- Provide supplemental oxygen, if available. (maintain SpO2 >90%)
- Maintain normal body temperature
- Ensure hydration
- Use gravity-assisted positioning (e.g., sitting upright to ease breathing).
Aftercare
(Primary Goals: Observation, continued oxygen support, gradual acclimatization)
Post-HAPE recovery is typically simple but crucial. Standard care includes: Supplemental oxygen (for up to 24 hrs) + bed rest + staying at the same altitude. If the issue is persistent, then the medical centres adopt the following methods:
- Nifedipine therapy for mild HAPE: Lowers systolic pulmonary artery pressure by up to 50% and improves oxygenation.
- 60 mg daily dose of nifedipine if symptoms remain unresponsive to rest and oxygen (Swenson, 2010).
- Mechanical ventilation + tracheal intubation, aiming to maintain SpO₂ > 90% (Gill et al., 2018).
Not HAPE then WHO? Differential Diagnoses
HAPE isn’t the only threat at high altitude. Several other illnesses can mimic its warning signs, including breathlessness, chest pain, or low oxygen. Before assuming it’s only HAPE, consider these common lookalikes:
| Differential Diagnoses | Possible Reason | Mimicked Symptoms |
| Asthma | Tight airways block breathing | Wheezing, short breath, chest tightness |
| Bronchitis | Lung tubes are swollen and irritated | Cough, breathlessness, chest discomfort |
| Mucous Plugging | Sticky mucus blocks airways | Sudden breathlessness, low oxygen |
| Myocardial Infarction | A heart attack limits blood flow | Chest pain, breathlessness, and sweating |
| Pneumonia | Lungs filled with infection | Fever, cough, chest pain, fatigue |
| Pneumothorax | Air escapes, lung collapses suddenly | Sharp chest pain, fast breathing |
| Pulmonary Embolism | Clot blocks the lung’s blood flow | Sudden breathlessness, chest pain |
| Upper Respiratory Tract Infection | A cold virus blocks the breathing tubes | Sore throat, cough, mild fever |
The Final Take
As a nature enthusiast myself, here’s my two cents on HAPE: If you suspect it, even slightly, descend! Contact your HDT (Himalayan Dream Treks) representative without hesitation or panic. Tell them you think it’s more than just AMS. They’ll know what to do and guide you toward the best course of action.
HAPE is the deadliest high-altitude illness, caused by hypoxia-induced hypoxemia that can lead to pulmonary edema. It’s serious, but also reversible. Remember what triggers it: high altitude, low oxygen, overexertion, and lack of acclimatization.
So, the best approach? On your part: Less panic, more trust. On your trek team’s part: Less fear, more action. You act promptly. Your trek team responds effectively.
In most treks across Uttarakhand and Himachal, descent is feasible and often just a few hours away. But time is critical. The longer you “push through,” the worse it gets.
Take risks, not fatal ones.
FAQs
1) What is the fastest way to treat HAPE?
The fastest way to treat HAPE is to descend as much as possible. Descending with a combination of oxygen therapy through a mask works wonders. The least recommended descent at a time is 1000 m. Additional points to keep in mind are not to let the patient walk down because exertion leads to hypoxia, and thus, edema builds frequently, escalating severe issues. The patient should be placed on a folding stretcher, keeping their body at rest.
2) Can HAPE affect children and older adults?
Yes. HAPE does not discriminate by age. Children, teens, adults, and older adults are all equally at risk.
Note: Some studies suggest that males may be more prone, possibly due to differences in activity levels or physiological factors.
3) Are there any emergency medicines I can carry for HAPE?
The emergency medicine options for HAPE include nifedipine (which reduces pulmonary pressure), sildenafil (which improves blood flow in the lungs), and dexamethasone, which reduces inflammation (more effective for HACE but sometimes helpful in HAPE as well). Before drug use, make sure to consult an on-trek expert.
4) Is HACE more fatal than HAPE?
HACE is more severe neurologically and often considered more fatal.
But more people die of HAPE, mainly due to late detection and delayed treatment, not necessarily because it’s inherently worse.
5) How can I prevent HAPE if I’ve a history of altitude sickness?
The preventive measures for HAPE, if you have a history of altitude-related sickness, include graded ascent and ample time to acclimate. You’ll also benefit from keeping your sleeping altitude only 350 m (max) above the sleeping altitude before it. Lastly, consider prophylactic meds if prescribed.
6) What altitude typically triggers HAPE symptoms?
HAPE is usually triggered within 2-5 days of staying at an altitude above 2,500 m. However, rare cases have occurred as low as 2,000 m, especially with rapid ascent or predisposing factors.
References:
- Paralikar S. J. (2012). High altitude pulmonary edema-clinical features, pathophysiology, prevention, and treatment. Indian journal of occupational and environmental medicine, 16(2), 59–62. https://doi.org/10.4103/0019-5278.107066
- Bärtsch, P., Mairbäurl, H., Swenson, E. R., & Maggiorini, M. (2003). High altitude pulmonary oedema. Swiss medical weekly, 133(27-28), 377–384. https://doi.org/10.4414/smw.2003.09657
- Schoene, R. B. (2008). Illnesses at high altitude. Chest, 134(2), 402–416. https://doi.org/10.1378/chest.07-0561
- Oelz, O., Maggiorini, M., Ritter, M., Waber, U., Jenni, R., Vock, P., & Bärtsch, P. (1989). Nifedipine for high-altitude pulmonary oedema. Lancet (London, England), 2(8674), 1241–1244. https://doi.org/10.1016/s0140-6736(89)91851-5
- Bärtsch, P., Maggiorini, M., Ritter, M., Noti, C., Vock, P., & Oelz, O. (1991). Prevention of high-altitude pulmonary edema by nifedipine. The New England journal of medicine, 325(18), 1284–1289. https://doi.org/10.1056/NEJM199110313251805
- Maggiorini M. (2006). High altitude-induced pulmonary oedema. Cardiovascular research, 72(1), 41–50. https://doi.org/10.1016/j.cardiores.2006.07.004
- Maggiorini, M., Brunner-La Rocca, H. P., Peth, S., Fischler, M., Böhm, T., Bernheim, A., Kiencke, S., Bloch, K. E., Dehnert, C., Naeije, R., Lehmann, T., Bärtsch, P., & Mairbäurl, H. (2006). Both tadalafil and dexamethasone may reduce the incidence of high-altitude pulmonary edema: a randomized trial. Annals of internal medicine, 145(7), 497–506. https://doi.org/10.7326/0003-4819-145-7-200610030-00007
- Rathi, U., Gill, R. K., Saroa, R., & Saxena, P. (2018). Essence of time in high altitude pulmonary edema–A case report. Saudi Critical Care Journal, 2(3), 48-50. https://doi.org/10.4103/sccj.sccj_31_18
- Kurtzman, R. A., & Caruso, J. L. (2018). High-Altitude Illness Death Investigation. Academic forensic pathology, 8(1), 83–97. https://doi.org/10.23907/2018.006
- Maggiorini M. (2006). High altitude-induced pulmonary oedema. Cardiovascular research, 72(1), 41–50. https://doi.org/10.1016/j.cardiores.2006.07.004
- Koul, P. A., Khan, U. H., Hussain, T., Koul, A. N., Malik, S., Shah, S., Bazaz, S. R., Rashid, W., & Jan, R. A. (2013). High altitude pulmonary edema among “Amarnath Yatris”. Lung India: official organ of Indian Chest Society, 30(3), 193–198. https://doi.org/10.4103/0970-2113.11625
- SINGH, I., KAPILA, C. C., KHANNA, P. K., NANDA, R. B., & RAO, B. D. (1965). HIGH-ALTITUDE PULMONARY OEDEMA. Lancet (London, England), 1(7379), 229–234. https://doi.org/10.1016/s0140-6736(65)91520-5
- Wu, T. Y., Ding, S. Q., Liu, J. L., Jia, J. H., Chai, Z. C., & Dai, R. C. (2012). Who are more at risk for acute mountain sickness: a prospective study in Qinghai-Tibet railroad construction workers on Mt. Tanggula. Chinese medical journal, 125(8), 1393-1400. https://doi.org/10.3760/cma.j.issn.0366-6999.2012.08.006
- Taylor, A. T. (2011). High-altitude illnesses: physiology, risk factors, prevention, and treatment. Rambam Maimonides Medical Journal, 2(1), e0022. https://doi.org/10.5041/RMMJ.10022
- Pennardt A. (2013). High-altitude pulmonary edema: diagnosis, prevention, and treatment. Current sports medicine reports, 12(2), 115–119. https://doi.org/10.1249/JSR.0b013e318287713b
- Mounier, R., Amonchot, A., Caillot, N., Gladine, C., Citron, B., Bedu, M., … & Pialoux, V. (2011). Pulmonary arterial systolic pressure and susceptibility to high altitude pulmonary edema. Respiratory physiology & neurobiology, 179(2-3), 294-299. https://doi.org/10.1016/j.resp.2011.09.011
- Luks, A. M., & Swenson, E. R. (2007). Travel to high altitude with pre-existing lung disease. The European respiratory journal, 29(4), 770–792. https://doi.org/10.1183/09031936.00052606
- Paralikar, S. J., & Paralikar, J. H. (2010). High-altitude medicine. Indian journal of occupational and environmental medicine, 14(1), 6–12. https://doi.org/10.4103/0019-5278.64608
- Modesti, P. A., Vanni, S., Morabito, M., Modesti, A., Marchetta, M., Gamberi, T., Sofi, F., Savia, G., Mancia, G., Gensini, G. F., & Parati, G. (2006). Role of endothelin-1 in exposure to high altitude: Acute Mountain Sickness and Endothelin-1 (ACME-1) study. Circulation, 114(13), 1410–1416. https://doi.org/10.1161/CIRCULATIONAHA.105.605527
- Singhal, S., & Alasinga, B.S. (2020). Delayed-onset high-altitude pulmonary edema: A series of 8 patients. Environmental Disease, 5(2), 52–52. https://doi.org/10.4103/ed.ed_1_20
- Khan, I. D. (2012). Extreme altitude pulmonary oedema (EAPO) in acclimatized soldiers. Medical journal, Armed Forces India, 68(4), 339–345. https://doi.org/10.1016/j.mjafi.2012.04.018
- Johnson, T. S., Young, J. B., & Landsberg, L. (1981). Norepinephrine turnover in the lung: effect of cold exposure and chronic hypoxia. Journal of applied physiology: respiratory, environmental and exercise physiology, 51(3), 614–620. https://doi.org/10.1152/jappl.1981.51.3.614
- Luks, A. M., McIntosh, S. E., Grissom, C. K., Auerbach, P. S., Rodway, G. W., Schoene, R. B., Zafren, K., Hackett, P. H., & Wilderness Medical Society (2010). Wilderness Medical Society consensus guidelines for the prevention and treatment of acute altitude illness. Wilderness & environmental medicine, 21(2), 146–155. https://doi.org/10.1016/j.wem.2010.03.002
- Broaddus, V. C., Mason, R. J., Ernst, J. D., King, T. E., Lazarus, S. C., Murray, J. F., Nadel, J. A., Slutsky, A. S., & Gotway, M. B. (Eds.). (2016). Murray & Nadel’s textbook of respiratory medicine (Sixth edition). Saunders, an imprint of Elsevier Incorporated. https://onesearch.nihlibrary.ors.nih.gov/permalink/01NIH_INST/g83mj/alma991001237582904686
- Swenson, E. R. (2010). High-altitude pulmonary edema. Textbook of pulmonary vascular disease, 871-888. https://link.springer.com/chapter/10.1007/978-0-387-87429-6_61
- Jensen JD, Vincent AL. High Altitude Pulmonary Edema(Archived) [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430819/
- High-Altitude Pulmonary Edema (HAPE): Causes & Treatment. (2024, October 21). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/high-altitude-pulmonary-edema
- Swenson, E. R. (2010). High-Altitude Pulmonary Edema. Textbook of Pulmonary Vascular Disease, 871–888. https://doi.org/10.1007/978-0-387-87429-6_61
- Deweber, K., & Scorza, K. (2010). Return to activity at altitude after high-altitude illness. Sports health, 2(4), 291–300. https://doi.org/10.1177/1941738110373065
- Baniya, S., Holden, C., & Basnyat, B. (2017). Reentry High Altitude Pulmonary Edema in the Himalayas. High altitude medicine & biology, 18(4), 425–427. https://doi.org/10.1089/ham.2017.0088
- Cremona, G., Asnaghi, R., Baderna, P., Brunetto, A., Brutsaert, T., Cavallaro, C., Clark, T. M., Cogo, A., Donis, R., Lanfranchi, P., Luks, A., Novello, N., Panzetta, S., Perini, L., Putnam, M., Spagnolatti, L., Wagner, H., & Wagner, P. D. (2002). Pulmonary extravascular fluid accumulation in recreational climbers: a prospective study. Lancet (London, England), 359(9303), 303–309. https://doi.org/10.1016/s0140-6736(02)07496-2
- Thareja, L. G. S., Chandra, B. A., Aggarwal, C. V., Uday, C. Y., Shekhar, L. C. A., Singh, L. C. K., … & Nair, L. G. V. (2025). NAMS task force report on high altitude. Annals of the National Academy of Medical Sciences (India), 61(1), 45-65. https://doi.org/10.25259/ANAMS_TFR_08_2024
- Walsh, B., & Agrawal, S. (2024). High-altitude Cerebral Edema and High-altitude Pulmonary Edema Diagnosed in the Desert: A Case Report. Clinical practice and cases in emergency medicine, 8(3), 202–205. https://doi.org/10.5811/cpcem.3851
- Burtscher, M., Hefti, U., & Hefti, J. P. (2021). High-altitude illnesses: Old stories and new insights into the pathophysiology, treatment, and prevention. Sports medicine and health science, 3(2), 59–69. https://doi.org/10.1016/j.smhs.2021.04.001
- Sartori, C., Allemann, Y., Duplain, H., Lepori, M., Egli, M., Lipp, E., Hutter, D., Turini, P., Hugli, O., Cook, S., Nicod, P., & Scherrer, U. (2002). Salmeterol for the prevention of high-altitude pulmonary edema. The New England journal of medicine, 346(21), 1631–1636. https://doi.org/10.1056/NEJMoa013183
- Deweber, K., & Scorza, K. (2010). Return to activity at altitude after high-altitude illness. Sports health, 2(4), 291–300. https://doi.org/10.1177/1941738110373065
- Berger, M. M., Schiefer, L. M., Treff, G., Sareban, M., Swenson, E. R., & Bärtsch, P. (2020). Acute high-altitude illness: Updated principles of pathophysiology, prevention, and treatment. Dtsch Z Sportmed, 71(11-12), 267-74. https://doi.org/10.5960/dzsm.2020.445
- Guyatt, G., Gutterman, D., Baumann, M. H., Addrizzo-Harris, D., Hylek, E. M., Phillips, B., Raskob, G., Lewis, S. Z., & Schünemann, H. (2006). Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians task force. Chest, 129(1), 174–181. https://doi.org/10.1378/chest.129.1.174
Leave a Comment